GEORGE NEWS - A snapshot from an average day in the George Hospital during the third wave of Covid-19 presents a harrowing picture.
Tasks include prioritising oxygen supply among patients and battling to coordinate beds to accommodate patients, says hospital CEO Michael Vonk, who has sent out an urgent plea to citizens to get vaccinated and so help ease the burden.
Vonk described a specific day in July on the Newzroom Afrika television channel to give the public an idea of what they have to cope with during the third wave.
"On this day, 41 staff were Covid positive. We try to operate our services, but at the same time a number of our staff are sick. On top of that we would have some staff that have been exposed and would have to quarantine. We had 89 Covid patients of whom 24 were in critical care, and that was our maximum; we couldn't take any more. And then we see what's happening in the community. The high, high incidence in the community, over 1 000 patients per 100 000,[means] this disease was everywhere. George and the Garden Route have been particularly hard hit during the third wave."
3 000kg of oxygen per day - R1m per month
Vonk said the Afrox truck delivers every one and half to second day. "In the last 30 days we've used 91 tons of oxygen - over 3 000kg per day. A massive increase to what we would use normally. I never thought I would ever be so excited to see the Afrox truck as I am."
The pandemic also has implications for employees other than frontline staff, such as workshop technicians who sometimes are called out in the night to de-ice the system because of the amount of oxygen being vaporised. At nearly R1-million per month, the financial cost spent on oxygen is massive.
Life and death decisions
One of the most difficult tasks is being part of the hospital ethics committee that has been meeting daily during the pandemic to prioritise and allocate critical care resources among patients. "Senior doctors, nurses, managers - both doctors on the frontline and doctors who are not working with Covid patients - come together. We use a standardised and evidenced-based tool (Western Cape critical care triage tool) to prioritise which patients will most benefit from critical care and who should have access to ventilators, and which patients will get high-flow nasal oxygen therapy. These are absolutely devastating decisions to make for the team. It's a decision no doctor should ever have to make alone," said Vonk.
The purpose of the committee is to share the responsibility for the decisions, so no one person has to make these independently. "It is to take the burden of decision-making away from solely the frontline staff, and to ensure that decision-making is fair and consistent. However, taking these decisions as a team does not necessarily ease the burden of those still having to implement the decisions."
He said sometimes they have to compare patients’ SOFA (sequential organ failure assessment) scores. "But this really allows us to standardise and it shows that there is fairness and equity and decisions are based on clinical research to maximise the benefit for the most patients."
If you're a patient in Beaufort West, Mossel Bay or George you have exactly the same access to critical care.
"We look to see how we can transfer patients between hospitals and work closely with hospitals across the whole district so we can manage our beds as a shared resource. This is one thing that has been immensely hard on some of the frontline staff - taking these life and death decisions."
No surgeries
During the successive waves of the pandemic the hospital has had to stop elective surgery and only operates on patients requiring emergencies and very urgent surgery. "We've converted our 18-bed day ward to a Covid ICU and have closed operating theatres. This has had a really big knock-on on non-covid patients waiting for operations. Some patients waiting from March last year have had their operations cancelled a number of times," said Vonk.
Delayed operations mean that patients wait in pain and discomfort for longer. Delaying surgery can mean that uncomplicated surgery can become more complex, sometimes with increased risk for patients.
"Patients presenting later and with more severe disease can mean longer operations, longer time to recover and longer hospital stays. This situation is being repeated across the country in both public and private hospitals."
Coordinating the available beds is a daily challenge . "The teamwork between different medical teams and the doctors and nursing staff has been absolutely outstanding. Daily they are looking to prioritise patients and coordinate the available beds. Just yesterday evening, there were 16 patients waiting for beds for admission and the team worked quickly together to see which patients they could send home and who they can bring back the next day."
Vonk said the current service pressures is something they do not want healthcare workers to go through again and the one thing that will change this, is if more people are vaccinated. Most people landing in the ICU or even general wards because of Covid-19 are unvaccinated.
Tourism industry must open up again
Vonk said the Garden Route is a tourist area and it is urgent to restore the livelihoods of residents. "We really need the tourists to be able to come back to the Garden Route, we need people to be able to provide jobs, we need our restaurants, we need our tourist industry to survive. My message to everybody on behalf of the hard-working teams at George Hospital and hospitals across the country, is that this (vaccination) is the one thing we can do as a country."
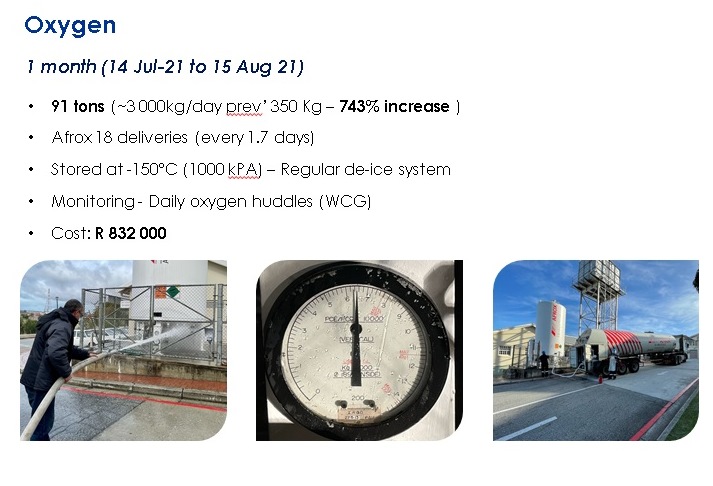 The Afrox truck's oxygen delivery every one and a half to two days is a welcome sight.
The Afrox truck's oxygen delivery every one and a half to two days is a welcome sight.
 Comparison of hospital admissions in the three waves.
Comparison of hospital admissions in the three waves.
 Comparing the active cases over time from the first to the third wave.
Comparing the active cases over time from the first to the third wave.
'We bring you the latest George, Garden Route news'